Research Suggests Good Oral Health May Reduce Risk of Cognitive Decline
Illustration by Jeannie Phan
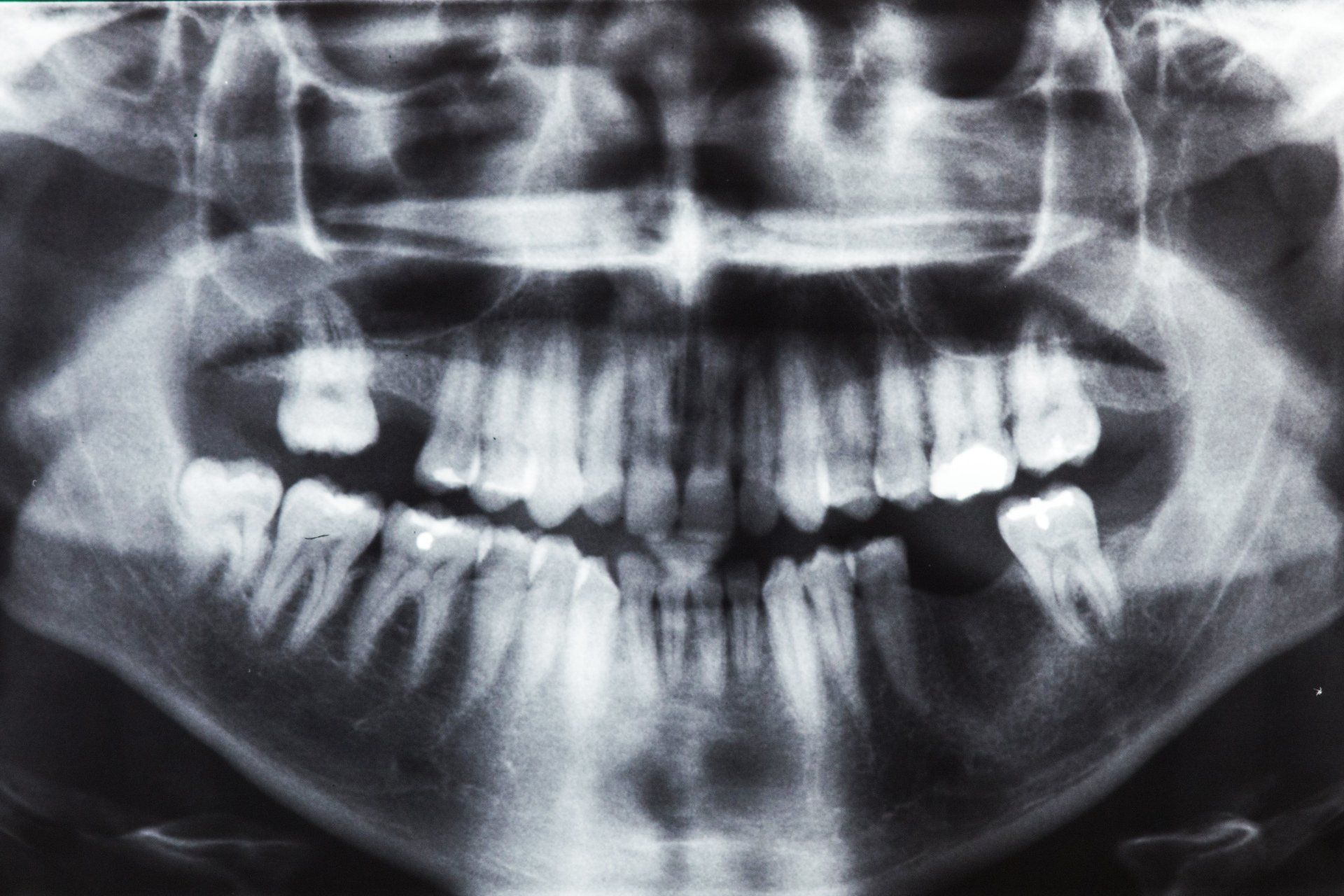
Going to the dentist may not be on everyone's list of favorite things to do, but results of recent studies are providing new reasons to make dental checkups a priority. A growing body of evidence links poor oral health, in particular gum disease, to a higher risk of Alzheimer's disease and other dementias. Mild gum disease (gingivitis) is when plaque and bacteria build up on the teeth and cause infection. A more advanced disease known as periodontitis can involve chronic inflammation that damages both the gums and the bone that anchors the teeth.
One study from Japan, published in Neurology in September 2023, for instance, found that periodontitis and tooth loss were associated with loss of volume in the hippocampus, a part of the brain involved in memory. To measure oral health, researchers counted each participant's teeth and probed their gums for signs of periodontitis. None of the participants—who were age 55 or older—had signs of cognitive decline at the time of their enrollment in the study. Each person had at least two MRI brain scans four years apart to detect any decrease in hippocampal volume.
The researchers found that having fewer teeth was associated with a faster rate of left hippocampal atrophy in subjects with mild periodontitis, while having more teeth was associated with a faster rate of atrophy in those with severe periodontitis. In other words, it wasn't enough to simply keep teeth. The key is having a mouth free of periodontal disease, says study author Satoshi Yamaguchi, DDS, PhD, associate professor at Tohoku University Graduate School of Dentistry in Sendai, Japan. Replacing missing teeth with good-fitting dentures helps maintain chewing function, which is important not only for good nutrition but also for brain health, he adds.
Researchers at Yale University likewise found an association between various indicators of poor oral health and brain health as measured on MRI scans. They analyzed data on more than 40,000 adults enrolled in the UK Biobank research project. Participants were screened for 105 genetic variants known to make people prone to getting cavities, losing teeth later in life, and requiring dentures. They also had MRI scans of their brains, which were examined for white matter hyperintensities, a sign of damage to the white matter of the brain. White matter lesions are seen as a possible indication of cognitive decline as well as gait and balance dysfunction, and may be associated with an increased risk of developing cerebrovascular disease, including stroke. The researchers also looked for changes in the microstructure of the brain.
In presenting their findings at the American Stroke Association International Stroke Conference last February, the researchers reported that people who were genetically predisposed to poor oral health were at higher risk for white matter hyperintensities and microstructural damage, both signs of decline in brain health. The authors will publish more detailed findings in a neurology journal in early 2024.
“The exact link isn't known yet. What we have are hypotheses,” says Cyprien Rivier, MD, MSc, the study's co-author and a postdoctoral fellow in neurology at the Yale School of Medicine in New Haven, CT. One theory is that the inflammation characteristic of gum disease “leads to the release of inflammatory factors throughout the whole body,” including the brain. Another theory suggests that poor oral health may allow bacteria from the mouth to reach the bloodstream. Once there, bacteria and their toxins could damage the blood-brain barrier, leading to increased inflammation in the brain, Dr. Rivier says.
Scientists agree that more research is needed to prove a cause-and-effect connection between oral health and brain health, including clinical trials demonstrating that improvements in oral health lead to measurable enhancements in brain health markers or a reduced risk of dementia and stroke, Dr. Rivier says. The question of whether there is a critical period in which poor oral health may impact the brain also is not known, although periodontal disease often occurs in midlife.
“We want to know how poor oral heath might affect the onset of dementia,” says Bei Wu, PhD, professor in global health and co-director of the Aging Incubator at New York University, who is seeking funding for a study to identify underlying mechanisms and pathways of oral health's effect on brain health.
Increased risk of heart attack and stroke also may be related to poor oral health. Dr. Wu believes that doctors, including neurologists, should be telling patients about the importance of good oral hygiene as part of overall disease prevention. Many dental ads focus on the cosmetic benefits, but Dr. Wu says keeping teeth and gums in good shape “is not just for beauty, it's for function.”
It's already well established that people with diabetes should get regular dental checkups because the disease can heighten the chances for gum disease. In some cases, dentists may flag the possible onset of diabetes because a patient's gums are red and swollen. A study Dr. Wu published in July 2023 in the Journal of Dental Research explored the interaction among dental disease, diabetes, and cognitive health in more than 5,000 people between the ages of 64 and 75 who were tracked for 12 years. Participants who had both diabetes and loss of teeth were at greater risk for worse cognitive function and faster cognitive decline than their counterparts who did not have diabetes or missing teeth, the study found.
People may not know they have gum disease because it doesn't always cause pain, especially in its milder forms. Telltale signs include red and puffy gums, sensitivity, bleeding while brushing, and the presence of “pockets” where the teeth meet the gums. (They are why dentists and dental hygienists press around the mouth with a probe.) Bad breath also may be a sign.
“Periodontitis can be a silent disease,” says June Sadowsky, DDS, MPH, professor at UTHealth School of Dentistry in Houston, so regular dental checkups are essential. In addition to the studies looking specifically at brain factors, there is evidence from epidemiologic studies that losing teeth is associated with having a shortened life span overall, adds Dr. Sadowsky.
“We don't want to scare people with a frightening message that if you have poor oral health, your brain is going to deteriorate,” Dr. Rivier says. But he hopes people respond to the idea that there might be added health reasons to adopt simple habits of daily brushing and flossing and regular dental checkups.
Making Care Accessible
As evidence on the connection between oral health and brain health continues to grow, the need to increase access to dental care is critical, says Dr. Wu. She is the senior author on a longitudinal study published in Research on Aging in 2019 that found that among people 50 or older in the United States, White people went to the dentist more often than Black or Hispanic people, and those born in the U.S. saw the dentist more often than those who were born elsewhere. Use of dentist services declined after age 80.
Barriers to getting dental care include lack of insurance coverage and possible scarcity of dental professionals in low-income communities, says Dr. Wu. Traditional Medicare does not pay for dental care, and even add-on policies may only partially cover fees.
For people with medical problems or just trying to get by, dental care may be a low priority, says Dr. Wu. But she says that the people at higher risk for heart and brain diseases may be exacerbating that risk because they don't have affordable or convenient access to dental care. “We need to raise awareness,” she says.
Research that linked data from the National Health and Nutrition Examination Survey to Medicare and National Death Index data found a strong association between periodontal disease in middle age and elevated risk for Alzheimer's disease and dementia-related death, says Cameron Jeter, PhD, a neuroscientist at the Kansas College of Osteopathic Medicine who studies oral health and brain health. She adds that some autopsy studies have found bacteria that is normally present in the oral cavity in the brains of people who had Alzheimer's disease.
“We're getting closer to understanding the causal links,” Dr. Jeter says, but she acknowledges that more research is needed. Still, she does not think it's a stretch to say that having poor oral health may decrease people's life spans and lower their quality of life.
“That should motivate people to pay attention to their oral health,” she says. “It should be a public health issue.”
Oral Health and Neurologic Disorders
“The relationship between the mouth and the brain is bidirectional,” says Cameron Jeter, PhD, a neuroscientist at the Kansas College of Osteopathic Medicine who studies oral health and brain health.
“Poor oral health, which includes teeth, gums, tongue, and inside the cheeks, can portend increased risk for future neurologic disease,” says Dr. Jeter, whose father had parkinsonism and struggled with oral health. But some neurologic disorders can interfere with proper care of one's teeth. People with dementia may not remember to brush their teeth. If that's the case, caregivers can place loved ones in front of a mirror, stand behind them, and reach around to do the brushing to make it feel as if the loved ones’ own hands are doing the work, she says. For those with tremor or muscle rigidity who have difficulty holding and using a toothbrush, adaptable toothbrushes may help.
People with neurologic conditions should tell their dentists about anything that may affect their oral health, says Seth Keller, MD, a New Jersey neurologist who is past chair of the American Academy of Neurology's section on adults with intellectual and developmental disabilities.
Many medications that treat neurologic conditions may cause dry mouth, for instance, which can increase the chances for developing cavities, Dr. Keller says. People with Parkinson's disease or other conditions that affect swallowing may drool or have trouble eating, which can result in poor nutrition and weight loss. Symptoms such as teeth clenching and mouth breathing, both of which can be bad for dental health, may result from any number of neurologic conditions, he adds.
For people with dementia or autism, a visit to the dentist may be frightening, but it's important to stay on top of dental health. Oral problems could cause discomfort or pain, which might exacerbate symptoms such as anxiety or depression. “Even with dementia, the mouth matters,” Dr. Keller says.
If people feel anxious about a dental checkup, they should seek out dentists who specialize in caring for people with certain disabilities, advises Dr. Keller. He also recommends scheduling appointments at the time of day best for loved ones, seeing the same dentist or hygienist every time, and discussing any concerns with the dental team beforehand.
CONTACT INFORMATION
Phone:
Fax:
(630) 834-8091
Address:
360 West Butterfield Road Ste 230 Elmhurst, IL 60126
BUSINESS HOURS
- Monday
- -
- Tue, Fri
- Closed
- Wed - Thu
- -
- Saturday
- -
- Sunday
- Closed
One Sat a Month
- Sunday
- Closed
- Mon - Sat
- Appointment Only
Other Days and Times Available by Appointment only.








In-Office Savings Plan
OUR LOCATION
CONTACT INFORMATION
Phone:
(630) 834-8088
Fax: (630) 834-8091
Email: info@radiantedentalspa.com
Address: 360 West Butterfield Road Ste 230 Elmhurst, IL 60126








In-Office Savings Plan
BUSINESS HOURS
- Monday
- -
- Tue, Fri
- Closed
- Wed - Thu
- -
- Saturday
- -
- Sunday
- Closed
One Sat a Month
- Sunday
- Closed
- Mon - Sat
- Appointment Only
Other Days and Times Available by Appointment only.
OUR LOCATION